Electronic Medical Records Employment Impacts
A large infusion of federal funds to support health information technology (HIT) development will likely alter the structure of the health care industry in Wyoming, as the health care delivery system evolves from paper records to electronic records. This paper highlights some of the relevant literature related to the history of electronic medical records (EMR) and electronic health records (EHR) as they relate to the state's employment structure and employment projections. Included are definitions of some basic terms found in HIT literature and descriptions of relevant federal laws related to HIT. This analysis looks at past research and opinions on the implementation and usage of EMR/EHR technologies and their potential workforce impacts. It also addresses the potential legal implications of a fully electronic medical record system and discusses EMRs in the context of modules used for billing and insurance system management.
Research & Planning (R&P) generally approaches the development of employment projections by studying past trends and incorporating present knowledge to forecast future events. Additional explanatory variables are also introduced into forecasting models to increase fit (closeness of forecast models to historical data). As a last step, the forecasts are checked against prior versions of state forecasts while taking into  account the unique features of the state and geographic areas within the state. Some unique properties of Wyoming and local areas include area dependence on certain industries such as oil & gas exploration and production, agriculture, local population, and educational attainment of state residents. The above factors and analysts' experience and knowledge combine to create a more or less "traditional" method of employment forecasting. Table 1 shows the general steps in this process.
account the unique features of the state and geographic areas within the state. Some unique properties of Wyoming and local areas include area dependence on certain industries such as oil & gas exploration and production, agriculture, local population, and educational attainment of state residents. The above factors and analysts' experience and knowledge combine to create a more or less "traditional" method of employment forecasting. Table 1 shows the general steps in this process.
These forecasting methods work well when the economy is not experiencing large shocks. What happens when an outside stimulus has the potential to radically change the employment structure? Normal methods may not apply and different methods may be required. Such may be the case in the health care industry due to the Health Information Technology for Economic and Clinical Health Act (HITECH) portion of the American Recovery and Reinvestment Act (ARRA) of 2009. A major focus of this legislation was to standardize electronic medical record information for all consumers nationally. In addition, considerable federal funding was designated to support implementation of this effort among health care providers.
Readers should also be aware that national implementation and usage of EMR/EHR is required by 2014 and is not optional. Section 3001(c) (3) (A) (ii) of the ARRA stipulates that an electronic health record is required for each person in the United States. Although our research focuses on institutions that voluntarily used EMR/EHR, universal adoption of the technology will be required in the near future.
Definitions and Nomenclature
-
EMR – Electronic Medical Record: information about individual transactions patients have with health care providers.
-
EHR – Electronic Health Record: an overview of EMR data from several locations. Ideally, it would be a top-level view of one's entire medical history including additions, corrections, and deletions of personal health information by patients.
-
ICD 9/10 – International Classification of Diseases: developed by the World Health Organization (WHO, 2010). "The ICD is the international standard diagnostic classification for all general epidemiological, many health management purposes, and clinical use." (http://www.who.int/classifications/icd/en/)
-
SNOMED-CT – Systematized Nomenclature of Medicine Clinical Terms: developed by the International Health Terminology Standards Development Organization (IHTSDO, 2010). "SNOMED CT aims to improve patient care through the development of systems to accurately record health care encounters. Ultimately, patients will benefit from the use of SNOMED CT, for building and facilitating communication and interoperability in electronic health data exchange." (http://www.ihtsdo.org/snomed-ct/)
-
HL7 – Health Level 7: A prominent method by which health information is exchanged between providers. "Health Level Seven International (HL7) is the global authority on standards for interoperability of health information technology with members in over 55 countries. HL7's vision is to create the best and most widely used standards in healthcare." (HL7 International, http://www.hl7.org/, 2010)
-
HIPAA – Health Insurance Portability and Accountability Act of 1996.
Relevant Law and National Developments
Medical positions geared toward information technology are not new. Malloy and Benoit (1998) discussed the development of a Director of Medical Informatics position. This job required a physician with substantial information technology (IT) credentials. Federal government initiatives in HIT are not unique to the ARRA. In 2004, President George W. Bush established the position of National Health Information Technology Coordinator (Executive Order 13335, 3 CFR 160 (2004)). In particular, Section 3 of the executive order states the coordinator's plan:
Advance the development, adoption, and implementation of health care information technology standards nationally through collaboration among public and private interests, and consistent with current efforts to set health information technology standards for use by the Federal Government (Subsection i).
The establishment of this office and the rules governing it were superseded when the HITECH Act passed as a portion of the ARRA. Within the HITECH Act, the Office of the National Coordinator for Health Information Technology was established (Section 3001). The responsibilities of the national coordinator included but were not limited to 1) certification of electronic health information use and exchange methods, 2) ensuring health information is secured and protected, and 3) coordinating federal HIT policy. In September 2010, it was reported that the United States Department of Health and Human Services (HHS) certified the first two technology review bodies authorized to test EMR systems (National Intelligence Report). Included in Section 3001 of the Act was funding to develop HIT infrastructure; Section 3012 provides for implementation assistance for health care institutions; and Section 3016 creates a program focused on training HIT workers who will implement a comprehensive system of electronic medical records. Among the institutions mentioned in the Section 3012 were HIT Regional Extension Centers. The purpose of these centers is to provide support to health care providers in their assigned regions with regard to the implementation of HIT in their operations. The regional extension center that covers Wyoming is located in Helena, MT (Harrington, 2010). This facility received a grant of $5 million to "…help doctors in Montana and Wyoming transition to electronic health records." The funds received by the extension center could be the first of many grants it may manage to facilitate EMR implementation in the region.
In addition to the regional extension centers, several community college consortia were developed to foster the education of information technology workers working in health care (United States Department of Health and Human Services, 2010). Although Wyoming stands to benefit from professionals trained by consortia, no Wyoming community colleges currently participate in the regional consortium. For a complete list of community colleges in the consortium, see http://healthit.hhs.gov/portal/server.pt/community/
healthit_hhs_gov__community_college_program/1804.
Private companies such as Microsoft and Google are showing interest in electronic health records also. Microsoft's Health Vault and Google's Google Health provide places for individuals to upload their medical histories. According to Mitchell (2008), one drawback to such storage services is that the data individuals place in them are not protected by the Health Insurance Portability and Accountability Act of 1996 (HIPAA; P.L. 104-191).
Educational Impacts
Although one may assume that all younger students have a high degree of technical sophistication, recent research has shown this is not necessarily the case. Lea, Pearson, Clamp, Johnson, and Jones (2008) discussed the challenges in preparing students for EMR usage. The authors found that wide disparities exist even in younger students' level of IT sophistication. Wilson and Tulu (2010) found that in addition to learning the records management portion of EMR implementation, students also needed to be well-versed in nomenclature terminology (e.g., SNOMED, ICD) in addition to data transfer technologies such as HL7. Because there is a virtual cornucopia of systems available for EMR implementation, the challenge for learning institutions is to decide which system to use. Will students who are trained on one system have a disadvantage with an employer that uses another system?
The educational system is already responding to the EMR challenge. The June 2009 issue of the Medical Records Briefing cited an 8% annual increase in Health Information Baccalaureate enrollment and a 10% increase in graduates between 2006 and 2007. In 2009, more than 50 baccalaureate programs, 200 associate-level, and 5 master-level accredited HIT programs existed in the United States. The accreditation agency for these programs is the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM).
Lake Region State College in Devils Lake, N.D., recently began offering non-degree certificate programs for four HIT occupations: workflow redesign specialist, health IT trainer, technical software support, and clinician/practitioner consultant (http://www.lrsc.edu/programs/default.asp?ID=925#HITredesign).
For some facilities, EMR is a recruiting tool to obtain the best candidates to fill positions. According to Joch (2009), hospitals are now using EMR to lure program completers and graduates to their facilities. One selling point for physicians in particular is the ability to enter orders from their homes (via the Internet) without having to make additional trips to hospitals.
Workforce Occupational Impacts
How might the move toward a fully electronic medical record system affect occupational employment? One occupation mentioned frequently in the literature is medical librarians. Welton (2010) indicated that these jobs formerly involved hard-copy cataloging and filing, but now are at the center of integrating IT and health care. Although these positions are typically located at teaching hospitals, the integration and management of electronic record systems may require the addition of such professionals in Wyoming's health care system. In another study (Larkin, 2010) the author estimated that an additional 51,000 HIT professionals would be needed between 2007 and 2012. Larkin also stated that workers must have extensive health care knowledge prior to employment. The author also cited a "short supply" of medical/nursing information officers.
Larkin found that smaller, rural hospitals often band together into co-operatives to share the costs associated with EMR implementation. At the time of the study, General Electric found that nearly 90% of its small and rural hospital customers prefer to completely outsource all IT functions. Spetz (2009) also found that small and rural hospitals struggle with EMR implementation. Staff had to be retrained to use IT systems, and facilities did not have the resources to allocate overtime or obtain nursing agency help as larger facilities. Palacio, Harrison, and Garets (2010) noted that urban hospitals were much more likely than rural hospitals to adopt EMR. For those who chose to adopt EMR, systems disparity was a barrier to interoperability. In 2003, more than 264 different EMR systems were in use but only 0.4% of physicians used the same software. The authors also found that the initial startup of an EMR system generally resulted in a loss in productivity of around 15% to 30% due to training time, nursing agency assistance, learning effects, temporary hiring, and other costs. However, the authors also noted that "over the long-term, clinical information systems improve efficiency while reducing resource utilization and unnecessary provider visits." Moreover, it is not clear to what extent productivity during implementation was negatively affected by the lack of HIT staffing. As EMR systems become common in the health care delivery system, the cost savings hypothesis can be empirically tested in a variety of health care settings.
One occupation growing with the implementation of EMR is nurse informaticists. These positions would be filled by licensed clinical nurses who obtain substantial HIT expertise (McIntire and Clark, 2009). Where the actual implementation of systems is concerned, Green & Thomas (2008) cited the need for "super users" to speed implementation. These individuals would be recommended by management and would receive in-depth training on systems. The drawback to the super users concept is that it may require extensive use of nursing agencies for coverage and substantial overtime during training periods. O'Brien (2006) also documented the presence of "super users" during EMR implementation. The author suggested that such users be available to staff for a minimum of 60 days after systems "go live." The hospitals in the study also found that each time a system upgrade occurred it was similar to starting over without EMR because of the additional overtime and nursing agency expenses. Although the hospitals in the study saved an estimated $50,000 in office supplies during the two years following implementation, the savings were more than offset by overtime and nursing agency expenses. The addition of staff is not specific to nurses and those who interact directly with patients. Chao, Twu, and Hsu (2005) stated that health care facilities will need to acquire additional information specialists to design systems to store and transmit EMR data.
EMR implementation is also challenging in long-term care (LTC) facilities. Phillips et al. (2010) found that EMRs were in very limited use in LTC settings. The authors stated that the adoption costs associated with EMRs do not appear to be offset by providers' cost savings. The facilities included in the study reported that cost was the primary deterrent to EMR implementation.
Table 2 summarizes our estimates of potential workforce impacts due to EMR implementation. Only estimates of 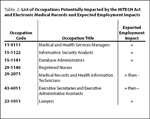 increasing or decreasing employment are shown. Occupations directly related to information technology in health care are projected to realize at least some employment growth due to additional demand for workers who have skills in the design, maintenance, and operation of medical record systems. More registered nurses will likely be required because some of these workers may become nurse informaticists and leave clinical practice. Also, nursing agencies may see increased demand during training and upgrade phases associated with EMRs. While demand for records technicians and administrative assistants will increase for a time as facilities transition to EMR, the demand for these occupations may decrease once systems become operational and reliable. Lastly, because of concerns about privacy, confidentiality, and information control, the demand for legal professionals with health and IT knowledge will likely increase.
increasing or decreasing employment are shown. Occupations directly related to information technology in health care are projected to realize at least some employment growth due to additional demand for workers who have skills in the design, maintenance, and operation of medical record systems. More registered nurses will likely be required because some of these workers may become nurse informaticists and leave clinical practice. Also, nursing agencies may see increased demand during training and upgrade phases associated with EMRs. While demand for records technicians and administrative assistants will increase for a time as facilities transition to EMR, the demand for these occupations may decrease once systems become operational and reliable. Lastly, because of concerns about privacy, confidentiality, and information control, the demand for legal professionals with health and IT knowledge will likely increase.
Cost and Quality of Care Impacts
The main selling points of EMR are the cost savings due to the reduction in paperwork and increases in the quality of care because medical errors are reduced. However, during this literature review, the results with EMR thus far have been mixed. Lea, Pearson, Clamp, Johnson, and Jones (2009) found that hospital length of stay tended to increase with EMR implementation. The authors surmised that shortcuts available to medical workers available in the paper system were being eliminated and their activities were being more accurately documented. Brokel (2009) noted that during implementation, considerable time and resources must be dedicated to record validation, particularly during the early phases of implementation which requires additional labor. The validation issue was also analyzed by Murphy, Oxencis, Klauck, Meyer, and Zimmerman (2009). In this study, the authors analyzed the use of EMRs in a pharmacy. The data capture and validation process in the pharmacy required the addition of 3.5 full-time equivalent (FTE) pharmacists. In a study of diabetic patients, Crosson et al. (2007) found that the presence of EMR did not increase quality of care. Here the authors posited that clinicians were successfully subverting the clinical decision rules built into the system in the interest of time savings resulting in a decline in their quality of care metrics. Retention of experienced staff is important to successful implementation. However, Robels (2009) cited a study by the Association of American Physicians and Surgeons which found that "…many physicians would rather retire than adopt EMRs."
Anderson (2008) noted that EMR is sometimes seen as "not ready for prime time" and that electronic systems are viewed as less effective than paper systems. Furthermore, confusing and conflicting government regulations have made it difficult for facilities to choose optimal systems. Hochstadt and Keyt (2009) found that while EMR will probably not save money, it will drive efficiencies in medical offices. Milton (2009) found that EMR introduction has not delivered on promised cost reductions. One of the major decisions health facilities must make is which data elements are to be retained. Milton also stated that people may self-ration services because of privacy concerns. The author noted that for-profit companies have begun to access electronic health data for analysis by their own internal health informatics experts. The author stated that in general, nurses and other health professionals require extensive IT training for successful EMR implementation.
The authors included in this review did not place considerable effort into determining the potential cost savings to patients as a result of EMRs. However, clinical research based on EMRs has garnered more attention. Pakhomov et al. (2007) discussed using EMRs to identify heart failure patients. The authors stated that, "the EMR may enable efficient case identification by providing access to clinical reports as soon as they become transcribed; however, novel methods of identification that use the EMR require rigorous validation" (p. 281). Patient EMRs were analyzed using two methods 1) natural language processing (text mining) of clinical notes and 2) predictive modeling. The authors noted that predictive modeling was more suited to clinical trials while natural language processing "may be more suitable for observational studies." (p. 287). This study was conducted at the Mayo Clinic, an institution that has used EMRs since 1994. In another study (Wilke et al., 2007) similar methods were used to identify subjects for a diabetes clinical research project. The work done by Wilke et al. (2007) also used natural language processing in addition to clinical notes and patient DNA data. Proper selection of research subjects using EMRs in these studies increased the efficiency of research dollars and likely produced more reliable results compared to studies where EMRs were not used.
Legal Issues
One obstacle to the use of EMRs is deciding who owns the data. Although hospitals and physicians would bear the cost of implementation, it appears a significant proportion of the benefits accrue to patients, insurance providers, and clinical researchers. One group of authors (Richardson, Hall, and Madjd-Sadjadi, Z.) suggested a method to speed EMR usage might be to store data in information warehouses similar to credit bureaus. The authors cautioned that with this approach, consumers would likely encounter errors similar to those found in their credit reports, but at least the same standards would exist for all participants in the system. Steward (2005) stated that the Department of Health and Human Services (HHS) is required to develop data management standards that follow the legal standards of HIPAA.
Other legal issues arising with EMR usage include the documentation of clinician activities and their inclusion as evidence in malpractice proceedings. McLean (2008) cited the use of EMRs to mine doctors' activities. In response to this, new rules of evidence are being developed which require additional expertise in EMR data for liability purposes.
The Billing and Insurance System
The proper coding and recording of medical events is essential to good cost control. Hoffman (2003) indicated that a potential benefit of EMR systems would be to stem losses involved in billing/collections." EMRs can also assist in detecting activities which are still costly in terms of billing. Seiber (2007) analyzed the phenomena of "code creep" in Medicaid and state employee health insurance billing. Code creep occurs when medical events are coded in such a way as to increase revenue streams. An example of this could be to code a patient's condition as more severe over time when the actual condition of the patient remains unchanged. The implementation of EMR could benefit the billing and health insurance system both in terms of accuracy and in the early detection and prevention of fraudulent billing practices.
Conclusion
The electronic medical record infrastructure in the United States is quite fragmented. A large number of data storage systems, transfer protocols, and security algorithms exist for these data. A goal of the HITECH Act was to establish standards for these systems that would eventually pave the way for a nationally interoperable electronic health record for all citizens. To accomplish this task, a tremendous amount of training and retraining must take place, in addition to filling open positions in health care with people who are skilled in health care and information technology. The impacts on Wyoming's labor market could be dramatic. The intent of this literature review was to place national events in the context of Wyoming's labor market to highlight what changes and challenges might occur as a result of federal legislation. Quantifying the impact on occupational projections is complicated by the fact that the best business solutions may be to add new IT skills to existing occupations initially and subsequently develop new specialized occupations as the health care system evolves.
Although the cost savings from EMRs to patients do not appear to be well documented, benefits to some providers because of reduced paperwork and error reduction could be significant. In addition, medical researchers already leverage the power of electronic records to select and monitor subjects in both clinical trials and observational studies. This practice may increase the efficiency of medical research.
Senior Economist Douglas W. Leonard can be reached at (307) 473-3811 or dleona@state.wy.us.
References
Anderson, C. (2008). The ins and outs of electronic medical records. Applied Clinical Trials (September). Pp. 50-56.
Brokel, J. (2009). Infusing clinical decision support interventions into electronic health records. Urologic Nursing 29(5). Pp. 345-352.
Chao, H., Twu, S., & Hsu, C. (2005). A patient-identity security mechanism for electronic medical records during transit and at rest. Medical Informatics and the Internet in Medicine 30(3). Pp. 227-240.
Crosson, J., Obman-Strickland, P., Hahn, K., DiCicco-Bloom, B., Shaw, E., Orzano, A., & Crabtree, B. (2007). Electronic medical records and diabetes quality of care: Results from a sample of family medicine practices. Annals of Family Medicine 5(3). Pp. 209-215.
Green, S., & Thomas, J. (2008). Interdisciplinary collaboration and the electronic medical record. Pediatric Nursing 34(3). Pp. 225-228.
Harrington, J. (2010, May 11). Mountain-Pacific Quality Health Foundation awarded $5M grant for records conversion. Helena Independent Record. Retrieved November 12, 2010, from http://helenair.com/business/local/article_21f2ef90-5cc4-11df-a873-001cc4c03286.html
Health Level 7 International (2010). Home page. Retrieved November 12, 2010 from http://www.hl7.org/
Hochstadt, B., & Keyt, D. (2009). Health care IT: Supporting cost efficiencies in tough times. Benefits Quarterly (2009Q4). Pp. 7-8.
Hoffman, J. (2003). The emergency department: Is there a way to stem the economic bleeding? Health Care Biller (July 2003). Pp. 3-5.
International Health Terminology Standards Organization (2010). SNOMED-CT. Retrieved November 12, 2010 from http://www.ihtsdo.org/snomed-ct/
Joch, A. (2009). Another way to seal the deal. Hospitals & Health Networks (April). Pp. 38-39.
Larkin, H. (2010). Who'll run your IT? Hospitals & Health Networks (February). Pp. 22-24, 33.
Lea, A., Pearson, D., Clamp, S., Johnson, O., & Jones, R. (2008). Using the electronic medical record within medical undergraduate education. Education for Primary Care 2008(19). Pp. 656-659.
McIntire, S. & Clark, T. (2009). Essential steps in super user education for ambulatory clinic nurses. Urologic Nursing 29(5). Pp. 337-342.
McLean, T. (2008). Electronic medical record metadata: Do you know what's in your record? Journal of Controversial Medical Claims 15(1). Pp. 16-18.
Medical Records Briefing (2009, June). HIM job market remains promising for new grads as national attention focuses on health IT. Pp. 6-9.
Milton, C. (2009). Information sharing: Transparency, ethics, and practice implications with electronic medical records. Nursing Science Quarterly 22(3). Pp. 214-219.
Mitchell, R. (2008). E-medical records: What seems to be the problem? Computerworld (July 14). Pp. 26-34.
Murphy, E., Oxencis, C., Klauck, J., Meyer, D., & Zimmerman, J. (2009). Medical reconciliation at an academic medical center: Implementation of a comprehensive program from admission to discharge. American Journal of Health-System Pharmacy 66(1). Pp. 2126-2131.
O'Brien, M. (2006). Implementation of the EPIC electronic medical record/physician order-entry system. Journal of Healthcare Management 51(5). Pp. 338-343.
Pakhomov, S., Weston, S., Jacobsen, S., Chute, C., Meverden, R., & Roger, V. (2007). Electronic medical records for clinical research: Application to the identification of heart failure. The American Journal of Managed Care 13(6). Pp. 281-287.
Palacio, C., Harrison, J., & Garets, D. (2008). Benchmarking electronic medical records initiatives in the US: A conceptual model. Journal of Medical Systems 34. Pp. 273-279.
Phillips, K., Wheeler, C., Campbell, J., & Coustasse, A. (2010). Electronic medical records in long-term care. Journal of Hospital Marketing and Public Relations 20. Pp. 131-142 .
Richardson, C., Hall, M., & Madjd-Sadjadi, Z. (2010). Lessons from credit bureaus for improving the market for electronic medical records. The Journal of Consumer Affairs 44(3). Pp 546-556.
Robels, J. (2009). The effect of the electronic medical record on nurses' work. Creative Nursing 15(1). Pp. 31-35.
Seiber, E. (2007, Summer). Physician code creep: Evidence in Medicaid and state employee health insurance billing. Health Care Financing Review 28(4). Pp. 83-93.
Spetz, J. (2009). Information technology implementation in a rural hospital: A cautionary tale. Journal of Healthcare Management 54(5). Pp. 337-347.
Steward, M. (2005). Electronic medical records: Privacy, confidentiality, liability. The Journal of Legal Medicine 26. Pp. 491-506.
United States Department of Health and Human Services (2010). Community college consortia to educate health information technology professionals in health care program. Retrieved November 12, 2010, from http://healthit.hhs.gov/portal/server.pt/community/
healthit_hhs_gov__community_college_program/1804
United States Department of Health and Human Services (2010). Initial EHR certification bodies named. Retrieved November 12, 2010, from http://www.hhs.gov/news/press/2010pres/08/20100830d.html
United States Government Printing Office (n.d.) American Recovery and Reinvestment Act of 2009 (Public Law 111-5). Retrieved November 12, 2010 from http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong_public_laws&docid=f:publ005.111.pdf
United States Government Printing Office (n.d.). Health Insurance Portability and Accountability Act of 1996. (Public Law 104-191). Retrieved November 12, 2010, from http://www.gpo.gov/fdsys/pkg/CRPT-104hrpt736/pdf/CRPT-104hrpt736.pdf
Valdes, I., Kibbe, D., Tolleson, G., Kunik, M., & Peterson, L. (2004). Barriers to proliferation of electronic medical records. Informatics in Primary Care 12(1). Pp. 3-9.
Welton, N. (2010, July). The University of Washington electronic medical record experience. Journal of Medical Librarians Association 98(3). Pp. 217-219.
Wilke, R., Berg, R., Peissig, P., Kitchner, T., Sijercic, B., McCarty, C., & McCarty, D. (2007). Use of an electronic medical record for the identification of research subjects with diabetes mellitus. Clinical Medicine & Research 5(1). Pp. 1-7.
Wilson, E.V., & Tulu, B. (2010). The rise of a health-IT academic focus. Communications of the ACM 53(5). Pp. 147-150.
World Health Organization (2010). International Classification of Diseases. Retrieved November 12, 2010 from http://www.who.int/classifications/icd/en/